On paper, everything looks fine.
The patient journey is mapped.
The team is trained.
The values are clear.
Then Tuesday happens.
A handoff is “mostly done.”
A patient waits. Nobody updates them.
A nurse spends 12 minutes chasing one piece of info.
A simple decision goes up three levels because no one is sure who can say yes.
Your teams care. They work hard.
And still, the experience breaks.
Not because people don’t want to do good work.
Because small friction points repeat all day, every day.
So here’s a faster start that doesn’t add weight to already stretched teams.
Look at five moments. Together. Calmly. Without blame.
Pick one place to act first.
Run one small test in 7 days.
That’s how you start closing the experience gap.
In healthcare and life sciences, effort is rarely the issue.
Setup is.
When the setup is unclear, good people compensate.
They patch. They chase. They “make it work.”
For a while, that looks like resilience.
Over time, it becomes the way things are done.
And once “the way things are done” becomes normal, it becomes culture.
Culture is not only the values you announce.
It’s what shows up in the small, repeated moments of work.
So the real question is not “Do we have the right values?”
It’s:
Where does the experience break most often, for patientsand for teams?
An Experience Gap Scan is a short team session thatmakes the gap visible in real work.
Simple. Useful. Respectful of time.
Pick a small mix of people who touch the moment you want tolook at:
You are not trying to be “representative.”
You are trying to be clear, fast, and honest.
10 min. Pick the real case
Choose one situation that felt slow, unclear, or frustrating.
20 min. Walk the moment step by step
Where did it slow down. Where did it confuse people. Where did it break.
20 min. Rate frequency and impact
What happens often. What costs trust, time, or energy.
10 min. Decide next steps
Pick one moment to fix first. Set 3 actions. Assign owners. Set a date.
One line goal you can use:
“By the end of this hour, we choose one moment to improve and agree howwe’ll test it.”
These are “mirror moments” because they hit patients andteams at the same time.
Fixing them improves both.
For each moment, ask:
Read more: AHRQTeamSTEPPS patient handoff tools (I PASS the BATON, I-SBAR)
Read more:
Harvard Business Review: What is psychological safety?
Harvard Business School Working Knowledge: psychologicalsafety, burnout, retention

Read more: Patient Safety Switzerland: practical tools for Just Culture and communication (PDF)
The most common failure mode is turning this into a list of27 issues.
If you try to fix everything, you fix nothing.
You also teach the team: “Here comes another project.”
So choose one moment using two criteria:
Then pick one test you can run in 7 days.
Not a big redesign. A test.
A test that makes life easier for teams and clearer forpatients.
That is how momentum starts.
Culture is not what you say in a town hall.
Culture is what happens in these moments, especially under pressure.
This is also where mid-level leaders have real leverage.They connect big values to small daily moves, in the team’s day-to-day.
When you improve one moment, two things happen:
That is culture change you can see.
If you want, send me two lines:
I’ll tell you which of the five moments I’d start with, andwhat a good 7-day test could look like.
P.S. If you are tired of “big culture programs,” this is theopposite. One real case. One hour. One test. One week.


AI is already inside hospital workflows. Learn how CEOs, COOs, CIOs, and CTOs can govern it in Switzerland and the EU, and build proof of control fast.

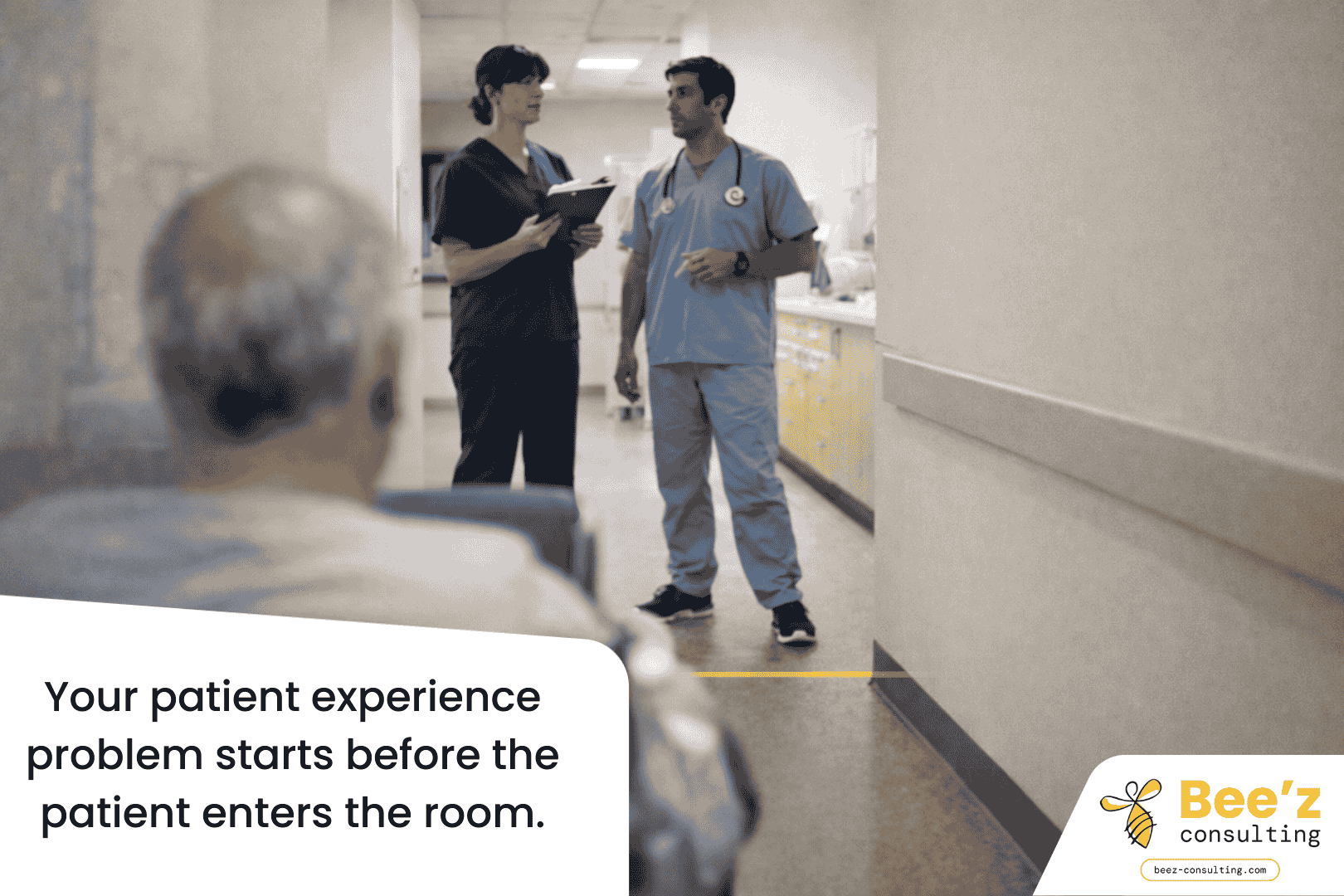
Patient experience starts before the bedside. Fix staff-to-staff handovers with two simple habits that cut friction, boost clarity, and build trust fast.

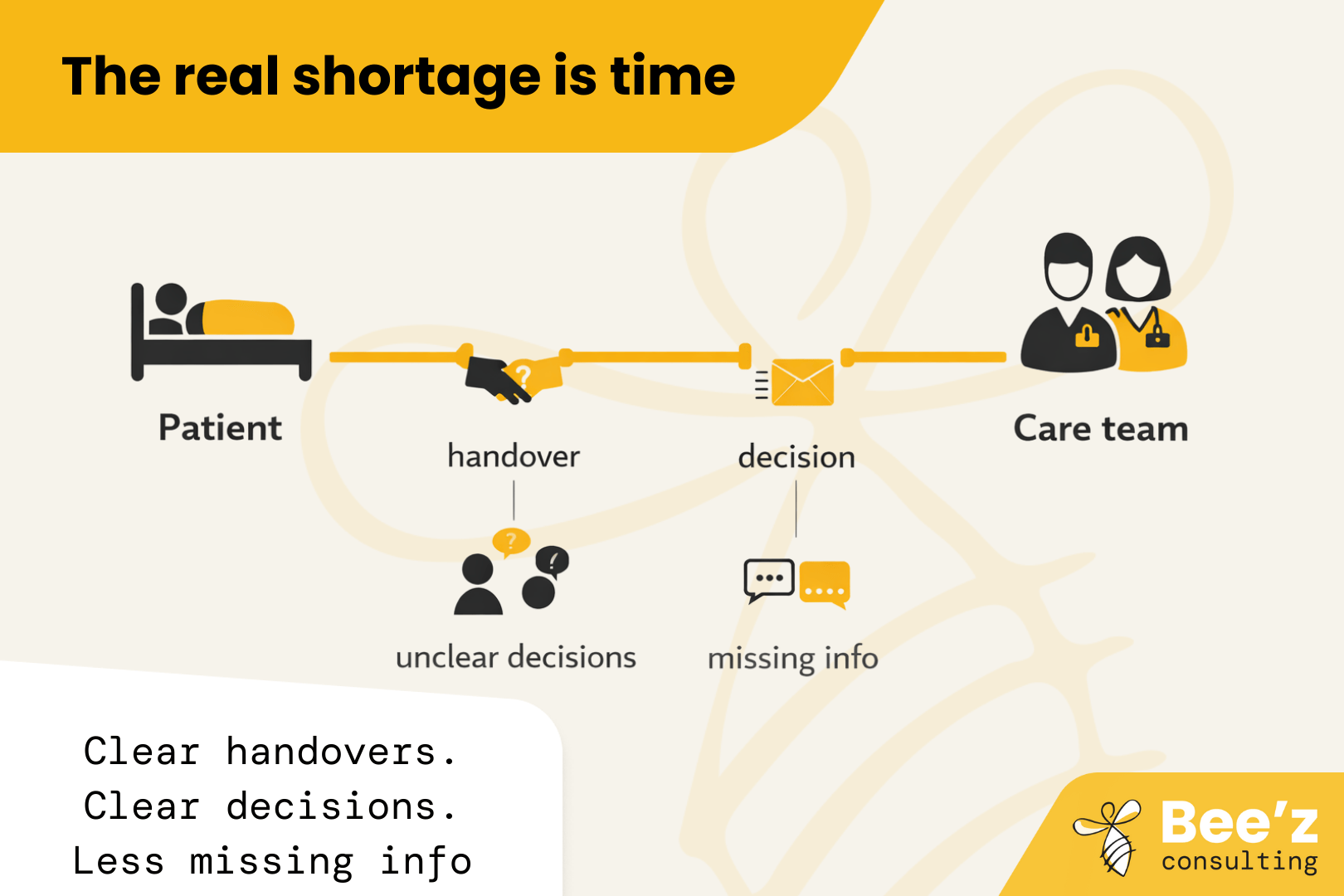
The real shortage is time with patients. “Thrive” is the missing lever. Fix daily workflow friction so hiring and retention finally pay off.
