It’s 09:17.
A patient is transferred from one unit to another. The nurse is kind, but rushed. The handover is half said, half guessed.
Two minutes later, the receiving team asks three basic questions that should have been answered already. The patient watches the back and forth. No one is rude. Still, the patient feels like a burden.
Most patient experience efforts focus on what happens between staff and patients. Scripts. Training. Surveys. Journey maps.
Those can help. But many of the real cracks start one step earlier. Between colleagues. In the handoff. In the tone. In the tiny gaps that feel normal because everyone is busy.
If this feels familiar, you likely have a staff-to-staff experience gap:
We see this pattern in clinics and hospitals of all sizes. The best teams don’t “try harder”. They hand off better.
The trap is thinking the fix must be big.
A new programme. A new dashboard. Another committee. Another push on “customer focus.”
Meanwhile, the handover stays the same. The cracks stay the same. The patient still feels the same thing.
A hospital can have strong values, strong intent, and strong clinical skill. And still create poor experience, simply because everyday coordination is brittle.
These two moves work because they are simple, repeatable, and rooted in real work. They do not add load. They remove wasted time.
You want a handover that still works when people are tired, stretched, and interrupted.
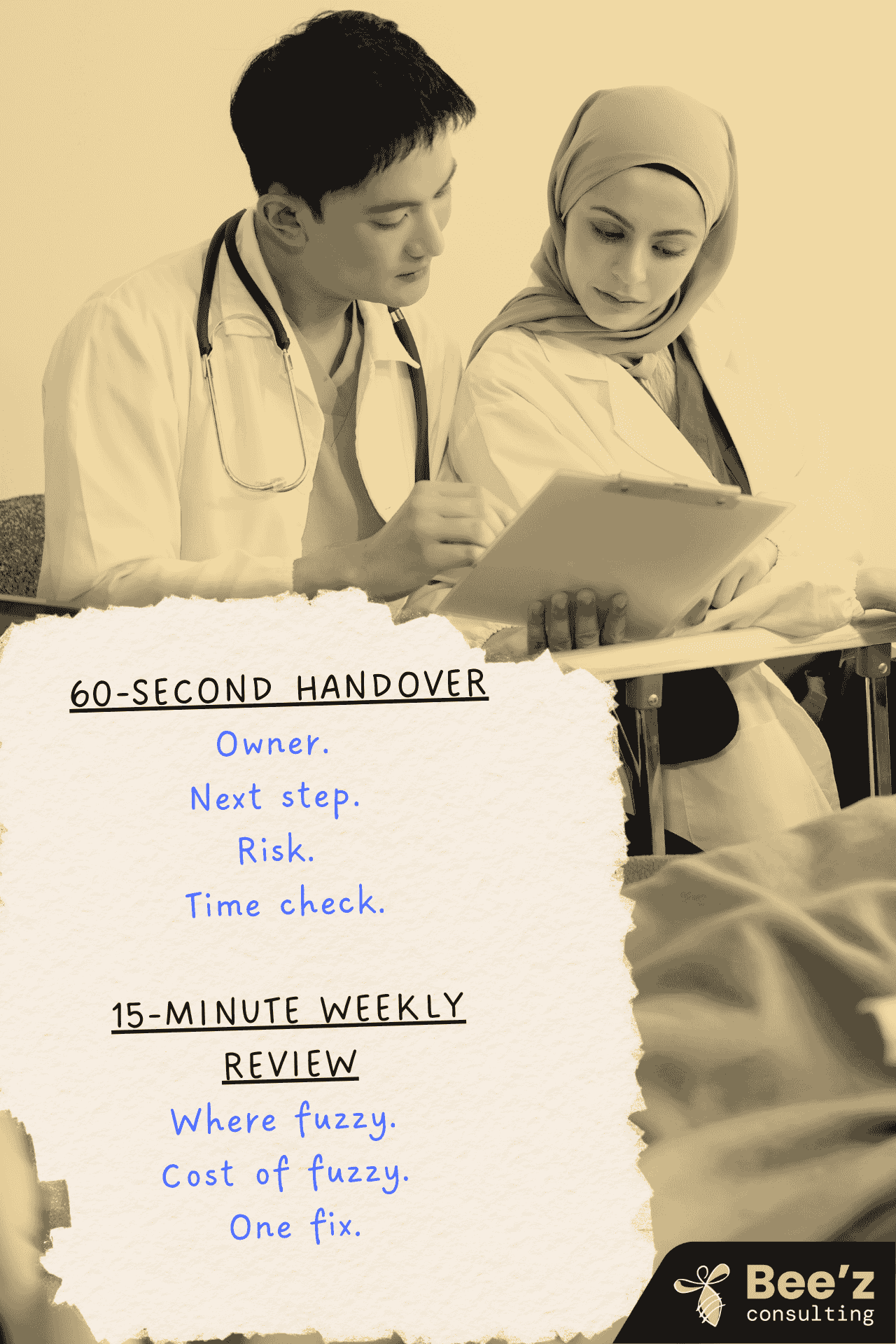
Use this structure:
If you cannot say it in 60 seconds, the handover is not ready.
If you want to make it stronger, add one closing line:
“What do you need from me to succeed in the next two hours?”
That line turns the handover from information transfer into ownership transfer.
Once a week, pick one real handover from the last seven days. Not the worst one. Not the best one. A typical one.
Do a 15-minute review with three questions:
Then stop. No big workshop. No blame. No long report.
Over time, teams stop saying “handover is always messy”. They start saying “handover is something we practise”.
You’ll notice:
Clear handovers also drive clearer ownership. Clear ownership drives faster decisions. Faster decisions reduce escalation and noise.
Patient experience improves because the system becomes more reliable. Not because people tried harder.
Pick one unit, one handover type, one shift pattern.
Run the 60-second handover rule for 10 days. Keep it light. Practice only.
At the end of the 10 days, do the weekly review once. Pick one handover. Choose one improvement. Then run another 10 days.
Where does clarity break first. Between teams, or at the bedside?
If you want to move fast on this, book a call with us.
We’ll help you identify the one handover type that creates the most downstream friction, then set up a short pilot your teams will actually use, without adding load.
In many hospitals we work with, the gap is not about effort. It’s about the handoff moment.
A “staff-to-staff experience gap” is the space between what the sending team thinks they passed on, and what the receiving team actually has in hand to act on.
It shows up when ownership is assumed rather than stated, when key context stays in someone’s head, or when the “next step” is not clear enough to execute. Patients may never hear the details.
They still feel the effects through delays, mixed messages, and uncertainty.
We often see this even in high-performing teams. Patients judge safety through reliability. Clinical care can be excellent, but if a team looks unsure, repeats questions, or gives slightly different answers, trust drops.
This is also well covered in patient safety work on handovers. The WHO flags handover communication as a known risk point and calls for clearer, more consistent handover practices. And when teams use a structured approach, results can improve. The I-PASS evidence base includes studies showing reductions in medical errors and adverse events after implementation.
So a fuzzy handover does not just create operational friction. It also creates uncertainty and stress cues that patients and families pick up quickly.
The patterns are usually easy to spot once you know what to look for. Common signals include:
When these patterns repeat, they become “normal.” That’s when they start shaping daily culture.
We keep it light and focused on real work. Typically, we:
This matches what the research shows about emotional culture. Change sticks when it’s built into repeated daily moments, not just explained once.
We recommend a simple spoken structure that teams can use even on a hard day:
If you want one extra line that increases ownership fast:
“What do you need from me to succeed in the next two hours?”
It sounds small. It reduces ambiguity, and that reduces stress cues in the moment.
We run a short, contained pilot that is easy to manage and easy to measure:

Patient experience starts before the bedside. Fix staff-to-staff handovers with two simple habits that cut friction, boost clarity, and build trust fast.

.png)
Leadership often breaks under pressure, not in training rooms. See why simulations help leaders practise real decisions and conversations, and how Bee’z Consulting turns practice into visible results within 7 days.

Close the experience gap fast. Run a 60 minute Experience Gap Scan to spot 5 friction moments and test one fix in 7 days. Clear owners. Better trust for teams.
