

“We’re stuck.”
The hospital’s leadership team sat in tense silence.
Across the table, employees’ representatives exchanged sceptical glances. A clinical director tapped his pen, barely hiding his frustration.
The facilitator’s question hung in the air:
“What will it take for us to move forward… together?”
They had spent months trying to “align stakeholders” around a sweeping care pathway redesign—intended to reduce bottlenecks and improve patient outcomes.
But each meeting seemed to deepen divisions.
Management accused clinicians of resisting change. Clinicians accused leadership of ignoring frontline realities. Employees’ representatives felt boxed out of key decisions.
Every “alignment” effort crumbled under the weight of distrust and conflicting priorities.
And yet—they had no choice but to collaborate.
The success of the transformation, and the future of patient care, depended on it.
This is the new leadership reality in healthcare and life sciences.
In times when change is accelerating, no single leader or organisation can drive transformation alone.
Whether redesigning care models, integrating new technologies, or shaping system-wide reforms—you must work with stakeholders who may not agree with you, trust you, or share your vision.
And this requires a new skillset.
Not conventional collaboration. Not “alignment” through force of will.
But something more adaptive, more courageous—and more uncomfortable.
Stretch collaboration.
In this article, we’ll explore why it is becoming a critical leadership skill for healthcare transformation—and how you can build it to drive real, sustainable change.
“If we just align stakeholders around a shared vision, we’ll succeed.”
It sounds reasonable. It’s taught in leadership programs. It appears in countless change management models.
But in today’s healthcare and life sciences ecosystems—this belief is quietly sabotaging many transformations.
Here’s why:
In complex, multi-stakeholder environments, alignment is imperfect and unstable.
You’re not dealing with one organisation. You’re navigating ecosystems of:
Each stakeholder group brings its own incentives, constraints, history—and emotions.
A “shared vision” may be aspirational.
But expecting perfect alignment around it creates false security—and dangerous blind spots.
Here’s the trap:
Meanwhile, unresolved tensions stay beneath the surface. When real decisions must be made—collaboration breaks down under the weight of unspoken disagreements.
Adam Kahane, in Collaborating with the Enemy, puts it clearly:
“We cannot change these situations unilaterally. We can only change them if we work with others.”
But—changing things together does not mean eliminating conflict.
The leadership shift required today is this:
→ From seeking false consensus → to building resilient collaboration across difference.
→ From trying to align everyone → to learning to collaborate with those you do not fully agree with or trust.
This is the heart of stretch collaboration.
And it’s the skill healthcare leaders now urgently need to master.
Healthcare transformation used to be seen as an internal challenge.
Restructure a hospital. Roll out a new clinical pathway. Introduce a digital tool.
Today? It’s an ecosystem challenge.

Transforming healthcare now means navigating:
No one actor controls the system.
And no one actor can “drive change” alone.
This creates an unprecedented leadership challenge. You must manage stakeholder ecosystems where:
✅ Interests diverge
✅ Incentives clash
✅ Power dynamics shift constantly
✅ Political and emotional tensions run high
In every healthcare transformation we support—whether hospital-based, biotech-driven, or system-wide—leaders tell us:
"It’s not the technical change that’s hardest. It’s the stakeholder dynamics.”
Why? Because today’s transformations are:
Managing this ecosystem requires a new level of relational skill.
Healthcare is becoming more polarised—inside and out.
Internally: generational divides, burnout pressures, value conflicts.
Externally: political overlays, societal expectations, equity debates.
Stakeholder engagement can no longer rely on assumed goodwill or “professional consensus.”
Leaders must engage across deep differences—sometimes with those who fundamentally challenge their worldview.
Each stakeholder brings different pressures:
Trying to “align” these interests around a single shared vision is often unrealistic.
The leadership task is not to eliminate divergence—but to navigate it constructively.
In this new reality, conventional stakeholder management—based on static stakeholder maps and consensus-building workshops—quickly hits its limits.
What’s needed is a more dynamic, adaptive, and courageous approach:
Stretch collaboration.
This dynamic isn’t limited to healthcare systems.
Across industries, leaders wrestle with relationship tensions, power imbalances, and clashing leadership styles — exactly the conditions where conventional alignment efforts break down.
For a powerful example of this in action, listen to this HBR Coaching Real Leaders episode, where an emerging leader navigates tension with a peer whose style is valued differently by senior leadership:
In the middle of that tense stakeholder meeting—the one where the hospital transformation seemed stuck—one leader finally voiced what others were thinking:
“We’re not going to agree on everything. Maybe that’s not the point.”
That was the turning point.
The shift from trying to force alignment… to building a way forward together, despite the differences.
Stretch collaboration is a leadership approach developed by Adam Kahane (Collaborating with the Enemy), for situations where:
✅ Stakeholders don’t fully agree
✅ There is a lack of trust
✅ Power is distributed and shifting
✅ The system is too complex for any single actor to control
Sound familiar?
This describes nearly every healthcare transformation today.
Kahane writes:
“We cannot change these situations unilaterally. We can only change them if we work with others.”

But working with others doesn’t mean pretending to agree—or waiting for full consensus before moving.
It means stretching your capacity to:
1️⃣ From control → to engagement
In conventional collaboration, leaders try to:
In complex healthcare transformations, this is not realistic.
Instead, leaders must engage stakeholders openly, acknowledging divergent perspectives and embracing the unpredictability of joint action.
2️⃣ From certainty → to experimentation
Traditional change programs often aim to design “the right solution” up front.
But in dynamic healthcare ecosystems, certainty is an illusion.
Leaders need to foster a culture of experimentation:
3️⃣ From self-righteousness → to co-responsibility
It’s tempting to think: “If only the other stakeholders would change, this would work.”
But stretch collaboration starts with a humbler question:
“What is my role in this situation—and how can I contribute to progress?”
Leaders who model co-responsibility build trust and unlock more authentic engagement from all sides.
In today’s healthcare and life sciences landscape:
Stretch collaboration is not a leadership luxury—it is becoming a core competency for anyone leading complex transformations.
And the good news?
It can be learned and practiced—starting now.
You maybe interested in reading this: Team Empowerment: The key to a bright future in Healthcare
A private hospital was embarking on an ambitious care pathway redesign.
The initiative was part of a wider national effort to reduce bottlenecks and improve patient outcomes. The mandate was clear. The goals were urgent.
Hospital leadership devoted months to developing a detailed new pathway model.
A project team was set up. Stakeholder meetings were scheduled—bringing together clinicians, managers, and employees’ representatives.
But as the conversations unfolded, tensions quickly surfaced.
Clinicians questioned whether the proposed pathways reflected frontline realities.
Employees’ representatives raised concerns about staffing levels and workload implications.
Managers worried about operational risks and resource constraints.
Each round of meetings seemed to deepen divisions.
Participation remained polite—but guarded. Progress was stalling.
Leadership tried the conventional responses:
They revised the vision.
They organised more alignment workshops.
They brought in external benchmarks to validate the model.
None of it shifted the underlying dynamics.
Trust was fragile. Stakeholder engagement remained surface-level. The project was at risk of losing momentum entirely.
Observing the situation, we advised leaders to reframe their approach—moving from ‘How do we get agreement?’ to ‘How do we make progress together?’
Workshops were reframed:
Instead of waiting for everyone to “agree”, the team moved forward by building trust through action:
Over time, new patterns of collaboration emerged:
✅ The redesigned care pathway was implemented in phases—adapted to real clinical contexts.
✅ Patient flow improvements were documented and shared.
✅ Staff engagement improved—as people saw their input reflected in concrete changes.
The breakthrough didn’t come from achieving consensus.
It came from learning to work with and through the system’s inherent tensions—stretching into a new way of collaborating across differences.
And that is precisely the kind of leadership capability healthcare transformations increasingly require.

One of the biggest shifts for healthcare leaders is reframing what “success” looks like in stakeholder management.
In complex transformations, full consensus is rare—and often not necessary.
The real goal is forward movement that incorporates diverse perspectives, even when not everyone agrees on every detail.
This means shifting leadership questions from:
❌ “How do we get everyone to agree?”
to:
✅ “How do we enable meaningful progress, despite our differences?”
This mindset opens new pathways for engagement and action.
In traditional change programs, tensions are often treated as problems to be smoothed over.
In stretch collaboration, tensions are valuable data.
They reveal the underlying concerns, needs, and unspoken risks that must be addressed for any transformation to succeed.
Healthcare leaders should create spaces where:
This builds trust and strengthens the resilience of the change effort.
You may be interested in reading this article as well: 5 Mind-Flipping Leadership Strategies That Will Transform Your Organization
It’s tempting to prioritise collaboration with the “easy” stakeholders—those who already share your views.
But healthcare ecosystems are too interconnected for selective collaboration.
Real progress requires working with those who bring uncomfortable perspectives—and with those you may not fully trust (yet).
This means:
Over time, this builds broader ownership and unlocks innovative solutions.
In dynamic healthcare environments, no single plan will be perfect from the start.
Leaders need to cultivate an iterative mindset:
This reduces risk, increases learning, and helps stakeholders see tangible progress—building momentum and credibility.
As Adam Kahane reminds us in Collaborating with the Enemy:
“The way forward is through joint action and joint learning—not through upfront agreement.”
Perhaps the most powerful lever is the leader’s own behaviour.
Stretch collaboration begins when leaders:
When leaders model this posture, it signals to all stakeholders that new forms of collaboration are possible.
And it transforms the tone of the entire change process—from one of opposition and control to one of shared ownership and learning.
Stretch collaboration is not just a way to “manage” complexity.
It’s a leadership skillset that unlocks real, measurable benefits for healthcare transformations.
Here’s what it makes possible:
When leaders engage across differences—instead of pushing for artificial consensus—they build deeper trust and ownership.
Stakeholders who feel heard and respected, even when they disagree, are more likely to:
This creates a more resilient base of support for transformation—one that can weather inevitable setbacks.
When tensions and divergent views are surfaced—not suppressed—new possibilities emerge.
Stretch collaboration enables:
The result:
More robust, fit-for-purpose outcomes that deliver real value in complex healthcare systems.
Ultimately, the goal of healthcare transformation is to improve patient outcomes.
When collaboration is authentic and inclusive:
This translates into better continuity of care, improved patient experience, and more equitable access to quality services.
Leaders who demonstrate the courage to collaborate across difference—and the humility to engage openly—build lasting credibility.
Their teams and stakeholders see them as:
This kind of leadership reputation is a powerful asset—both for the transformation at hand and for the organisation’s future.
Perhaps most importantly, stretch collaboration builds organisational muscle for future change.
Teams and stakeholders who learn to navigate complexity together become more:
In a healthcare landscape where change is constant, this kind of agility is invaluable.
In today’s healthcare and life sciences landscape, complexity is here to stay.
Stakeholder ecosystems will remain diverse, dynamic, and often divided.
In this reality, stretch collaboration is no longer optional.
It is a core leadership capability—for anyone seeking to drive sustainable transformation and improve patient outcomes.
Leaders who build this skillset will be better equipped to:
To close, here are a few questions for your next leadership team discussion:
Stretch collaboration is challenging.
It asks healthcare leaders to lean into discomfort, uncertainty, and complexity.
But it also opens the door to deeper engagement, more innovative solutions—and ultimately, better outcomes for patients and teams alike.
Are you ready to challenge the status quo and lead healthcare transformation with greater impact?
If you’d like to explore how stretch collaboration can accelerate change in your organisation, we’re here to help.
Connect with Bee’z Consulting today: www.beez-consulting.com/contact

Patient experience starts before the bedside. Fix staff-to-staff handovers with two simple habits that cut friction, boost clarity, and build trust fast.

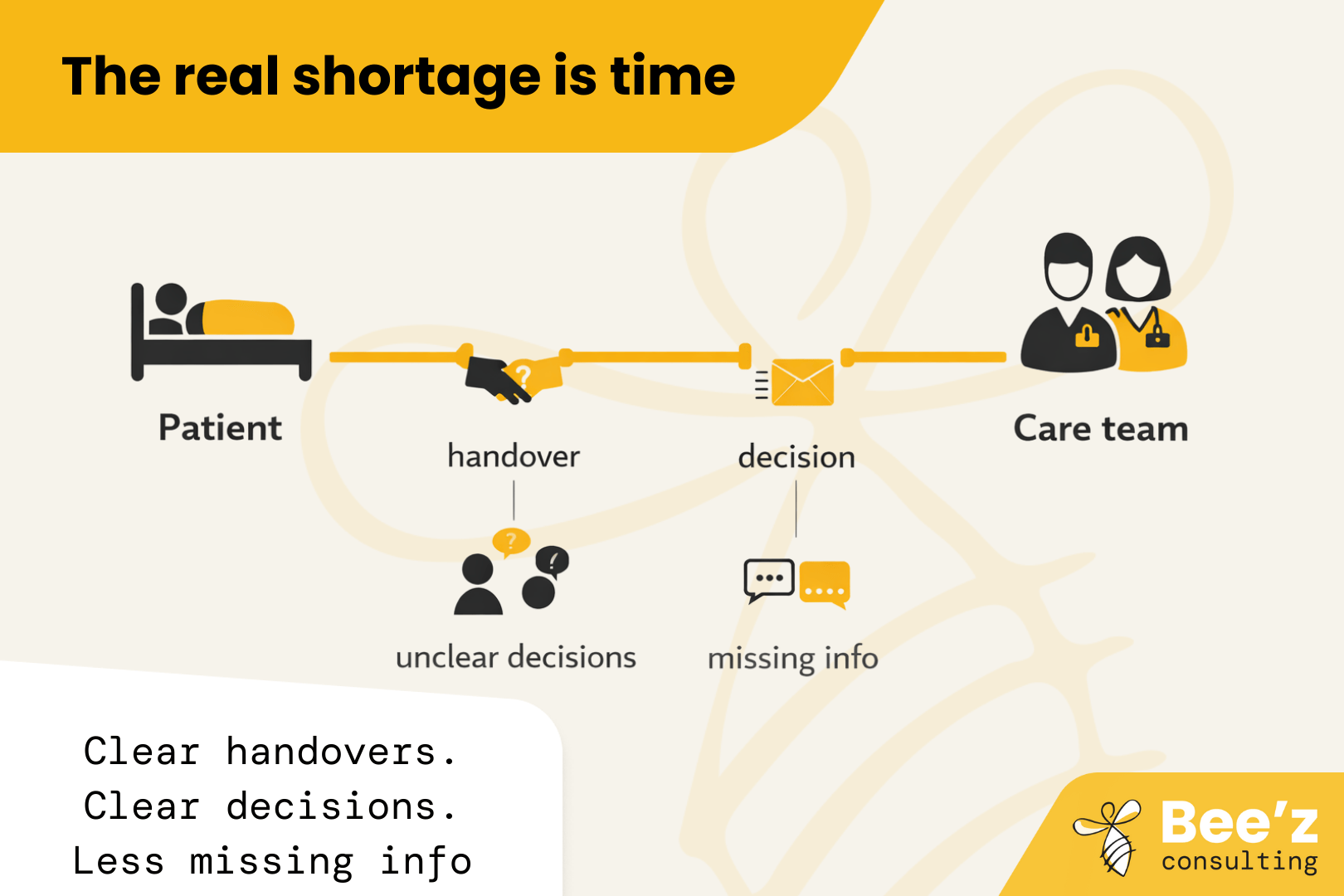
The real shortage is time with patients. “Thrive” is the missing lever. Fix daily workflow friction so hiring and retention finally pay off.

.png)
Leadership often breaks under pressure, not in training rooms. See why simulations help leaders practise real decisions and conversations, and how Bee’z Consulting turns practice into visible results within 7 days.
