
It’s 8:00am.
The boardroom is tense. Finance says: “We need to cut 10%.”
Clinicians reply: “If we cut, patients will suffer.”
Managers stare at the table.
The choice feels final.
This is the everyday reality of healthcare leadership: decisions framed as impossible trade-offs.
Either you save money or you save lives.
Either you protect staff or you deliver results.
Either you survive this year or you prepare for the next.
But what if those choices are false?
CFO vs. clinician.
Cut costs or harm care.
At the CHUV symposium on Value-Based Healthcare, leaders shared a different approach.
Instead of drowning in endless reports months too late, they measured what patients actually said mattered most — patient-reported outcome measures (PROMs).
Faster recovery, fewer unnecessary interventions, lower costs.
One team started small with just a single measure. That small win built trust.
Clinicians saw the benefit, patients saw better outcomes, leaders saw efficiency gains.
Only then did they expand.
Patients as partners was the real breakthrough. When patients helped design the measures, blind spots were exposed.
What mattered to them — like functioning at home after surgery — wasn’t always what doctors assumed.
Suddenly, “quality” was about life, not just length of stay.
A European clinic faced similar fears.
Leaders worried that introducing new governance rules would slow teams down.
Instead, by co-creating clear roles and aligning annual objectives with values, meetings focused better, handovers improved, and over time, patient satisfaction quietly rose.
Structure didn’t block care. It supported it.
Cost and quality are not enemies. Efficiency, when designed well, becomes a driver of excellence.
💬 Question for you: When did “cutting waste” in your organisationactually feel like better care for patients?
In crisis, leaders say, “Let’s survive this year. Transformation can wait.”
But in healthcare, there’s always another crisis. Survival mode becomes permanent.
Harvard Business Review’s On Leadership podcast, Episode 129 — Moving BeyondEither-Or Decision-Making — reminds us: stronger choices come when we ask not “Which one?” but “How do we do both?”
Survival and transformation don’t have to compete.
A global life sciences company under heavy regulatory pressure wanted to freeze leadership development. “Let’s deal with this first,” they said.
Together, we made a different choice: weaving leadership training into the crisis itself.
Through leadership simulations, managers practised:
These weren’t abstract skills — they were exactly what the crisis demanded.
People still felt stretched, but they saw that today’s emergencies could also be tomorrow’s practice ground.
Survival and transformation moved forward together.
Crisis isn’t the time to pause change. It’s the time to embed it.
Habits built under pressure stick.
💬 Question for you: During your last crisis, did your team only fightfires — or did you also plant seeds for the future?
“If we focus on wellbeing, performance will drop.”
But exhausted teams don’t perform. Healthy ones do.
Nearly three-quarters of healthcare executives report feeling burned out in thepast six months, and 93% say it’s hurting their organisations (source: AHA).
Burnout isn’t just a personal problem — it’s a performance crisis.
Wellbeing and performance are connected.
The same practices that support people often strengthen results.
At one healthcare provider, managers feared that investing in wellbeing would lower the bar.
Together, we introduced small team rituals and feedback habits.
The change wasn’t dramatic, but it was visible.
Energy came back into the room.
Performance improved because staff could focus on their work without fear of blame.
Wellbeing fuels performance. The two rise together.
💬 Question for you: What’s the smallest leadership habit you’ve seenthat lifted both wellbeing and results?
Harvard calls it integrative thinking.
We call it both-and leadership.
The clinic that learned structure could improve care and efficiency.
The pharma team that turned crisis into a training ground.
The healthcare organisation that discovered wellbeing and performance areallies, not rivals.
The breakthrough wasn’t a grand announcement. It was small, practical shifts.
Middle managers trying new habits.
Leaders reframing false choices.
Teams daring to connect opposites.
That’s what both-and leadership looks like in practice.
Executives may set the vision.
But it’s middle managers who bring it to life.
Research from MIT Sloan shows culture is built “from the middle out.”
Managers are the translators — turning big values into small daily actions.
At Bee’z, we’ve seen how quickly culture shifts when middle managers change the questions they ask, the rituals they build, and the way they hold accountability.
For more, see:
Middle managers are not the middle of the story. They are the bridge.
Every healthcare leader faces the same pressure points.
These are the traps that keep organisations stuck.
But here’s what the strongest leaders know:
Both-and leadership is not theory.
It’s practice.
And it’s happening now.
If your organisation is still stuck ineither-or debates, you’re not alone. Most are.
But the cost of waiting is high: staff attrition, wasted resources, lost trust.
The good news?
Moving beyond either-or doesn’t require a revolution.
It starts with practical steps: clearer roles, better questions, small rituals, tighter feedback loops.
We’ve seen it work.
We’ve helped leaders at clinics, hospitals, and life sciences organisations make these shifts.
And the payoff is real: healthier teams, stronger performance, and culturesthat feel alive.
Healthcare doesn’t have the luxury of false choices.
If your organisation is still stuck in either-or debates, you’re already behind.
Your teams feel it.
Your patients see it.
The shift to both-and leadership won’t wait — and neither should you.
At Bee’z, we help leaders make that shift — through:
👉 Let’s talk about how your organisation can move beyond either-or → www.beez-consulting.com/contact

Patient experience starts before the bedside. Fix staff-to-staff handovers with two simple habits that cut friction, boost clarity, and build trust fast.

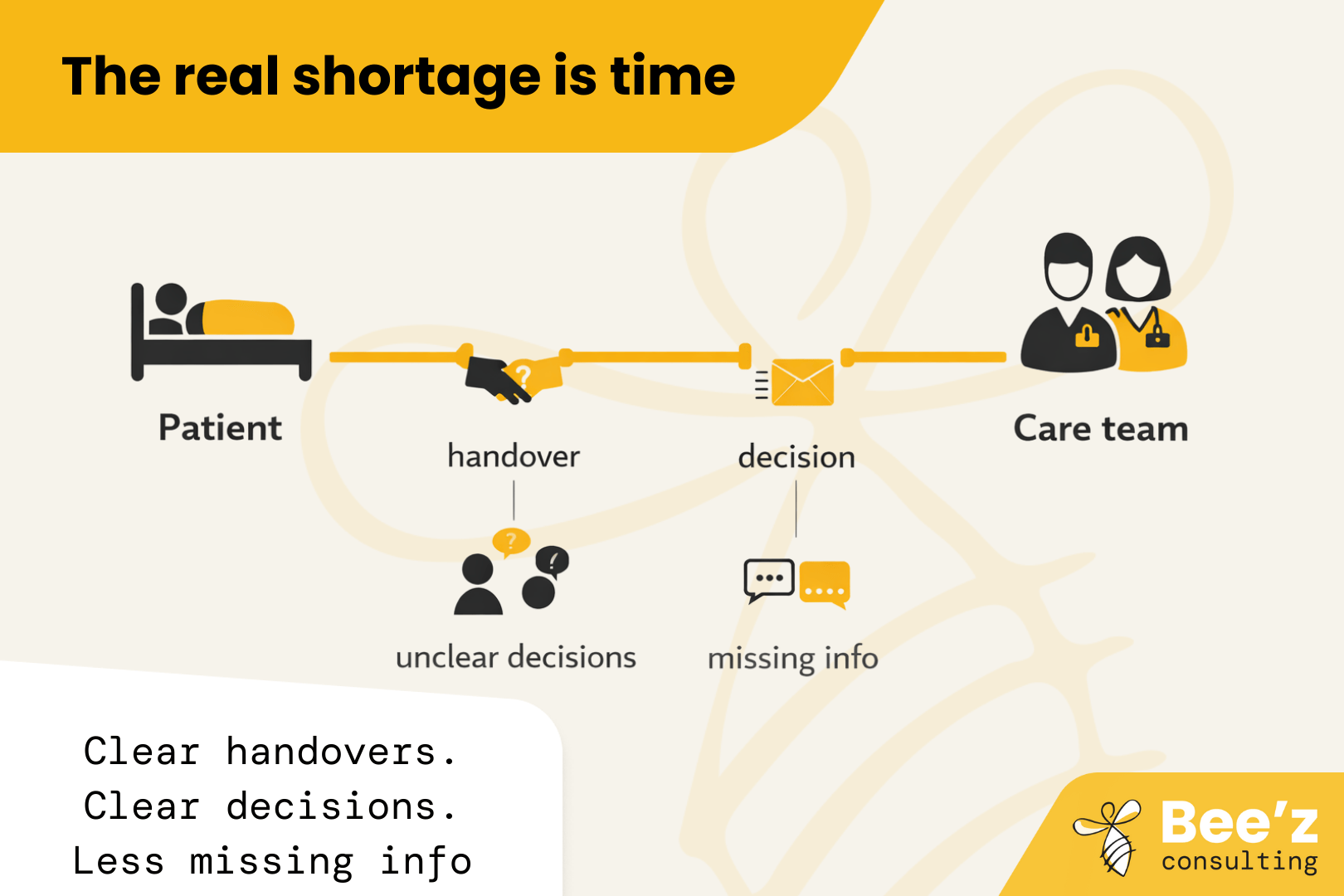
The real shortage is time with patients. “Thrive” is the missing lever. Fix daily workflow friction so hiring and retention finally pay off.

.png)
Leadership often breaks under pressure, not in training rooms. See why simulations help leaders practise real decisions and conversations, and how Bee’z Consulting turns practice into visible results within 7 days.
