
It’s 6 a.m. in Uri. The corridor lights come on.
A nurse rubs her eyes after a long night.
A young doctor checks the morning list.
Upstairs, the CEO scans the occupancy dashboard.
Three people, one question: how long can we keep doing more with less?
Across Switzerland, that question has become familiar. But amid the pressure, new answers are quietly emerging. Answers that reveal what kind of leadership the system needs next.
Swiss healthcare has long stood for quality and reliability.
But even strong systems bend under constant demand. Workforce shortages, financial constraints, and rising expectations are testing every hospital’s ability to adapt.
Swissmedic’s 2024 inspection report made this clear.
In 23 hospitals, inspectors found gaps in medical device management, maintenance, and cybersecurity.
Not because people stopped caring, but because the system leaves little time or space to improve.
Compliance takes energy.
Real quality takes collaboration.
Many teams are running on empty.
This tension between invention and impact was echoed at the Future Health Lausanne 2025 conference.
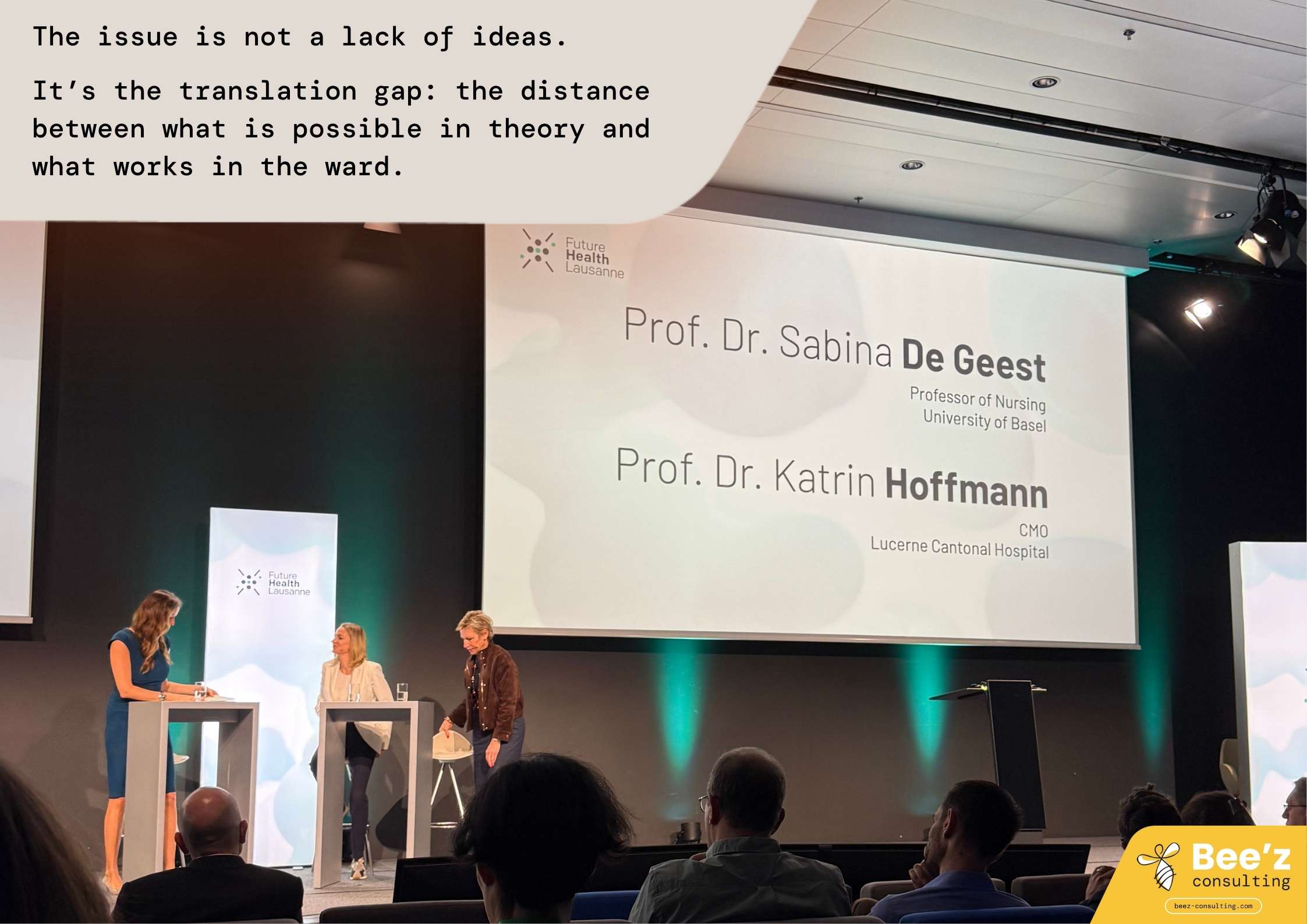
Professor Katrin Hoffmann, Chief Medical Officer at the Lucerne Cantonal Hospital Group, reminded the audience of a staggering truth:
“From bench to bedside, it used to take about 17 years for research to reach daily practice.
That cannot be. Innovation must move faster , and it must also fit the reality of hospitals and the people who work in them.”
Her point drew nods across the room.
The issue is not a lack of ideas.
It’s the translation gap — the distance between what is possible in theory and what works in the ward.
At the Kantonsspital Uri, CEO Fortunat von Planta kept the hospital profitable in 2024, even as occupancy swung between 55 and 147 percent.
His approach was simple but bold: trust the people closest to the work.

The hospital’s new collective labour agreement made flexible hours fair and transparent.
When patient numbers dropped, staff could go home early. When demand rose, they came back willingly.
Everyone understood the rules. Everyone shared the responsibility.
At the same time, the hospital became almost paperless, using digital tools and AI-assisted coding to avoid revenue loss.
But the biggest gain was not technical. It was cultural.
Flexibility became a shared rhythm rather than a source of frustration.
In Neuchâtel, Professor Philippe Eckert is rethinking what a hospital should be. As CEO of the Réseau Hospitalier Neuchâtelois (RHNe), he believes the future lies beyond the walls.
His team is creating decentralised health centres and mobile care units in geriatrics, rehabilitation, and palliative care.
The goal: follow patients across their entire journey, not just treat them during hospital stays.
This also supports staff.
By concentrating more care during daytime hours, RHNe lightens night and weekend workloads, giving professionals a more balanced rhythm of life.
The future of care is not inside hospitals. It is between them.
Swissmedic’s findings revealed the limits of compliance-driven quality.
Many hospitals meet minimum standards but struggle to go further.
Time pressure and under-investment play a role — but the deeper issue is fear.
When people fear being blamed, learning stops.
At Future Health Lausanne 2025, Professor Sabina De Geest, Professor of Nursing at the University of Basel and co-founder of the Swiss Implementation Science Network, called this “the missing middle of innovation.”
“We invest millions in research and trials, but very little in what happens next : how we bring innovation into real-world care. That’s the start of implementation science.”
Her message was clear: innovation is not only discovery, but disciplined translation — understanding context, involving stakeholders early, and building strategies for real adoption.
H+ and Swissmedic are now turning that philosophy into practice, co-developing peer-learning platforms where hospitals learn from each other’s near misses instead of hiding them.
Real quality grows when people feel safe to speak up — and learn.
At the same Lausanne panel, Professor Hoffmann shared a simple but powerful example.
Her team in Lucerne introduced an AI-assisted duty-scheduling app for nurses. However, instead of imposing it, they co-designed it with those who would use it.
The result? Higher satisfaction and three hours saved per scheduling cycle for each planner.
“It finally feels like the system works for us, not the other way around,” one nurse told her team.
It’s a small story, but it captures a larger truth: technology succeeds when it’s built with people, not for them.
Under Article 58a LAMal, Switzerland’s new Quality Convention is quietly creating a more collaborative system.
Hospitals are now part of national programmes on medication safety, sepsis prevention, and surgical safety.
The most symbolic example: the *“Room of Errors”* — a simulation space where teams explore real mistakes and what can be learned from them.
It’s not a place of blame, but of growth.
These initiatives mark a shift from inspection to introspection, turning compliance into community.
Because insight only matters when it turns into action — these are the mindsets shaping the next chapter of Swiss healthcare.
Swiss healthcare stands at a crossroads.
One path leads to more control, more reporting, and more exhaustion.
The other leads to partnership — across professions, institutions, and generations of caregivers who still want to make a difference.
The first path may feel safer.
The second will take courage.
But it’s the only one that can rebuild trust.
Transformation doesn’t begin with a new policy.
It begins in a conversation where people feel heard, in a team that learns instead of blaming, in a leader who chooses connection over perfection.
The question is no longer whether Switzerland can afford change.
It’s whether leaders can afford not to lead it, from the inside out.
Bee’z Consulting supports hospitals and healthcare organizations in developing cultures of trust, accountability, and collaboration that turn strategy into lived behaviour.


AI is already inside hospital workflows. Learn how CEOs, COOs, CIOs, and CTOs can govern it in Switzerland and the EU, and build proof of control fast.

Patient experience starts before the bedside. Fix staff-to-staff handovers with two simple habits that cut friction, boost clarity, and build trust fast.

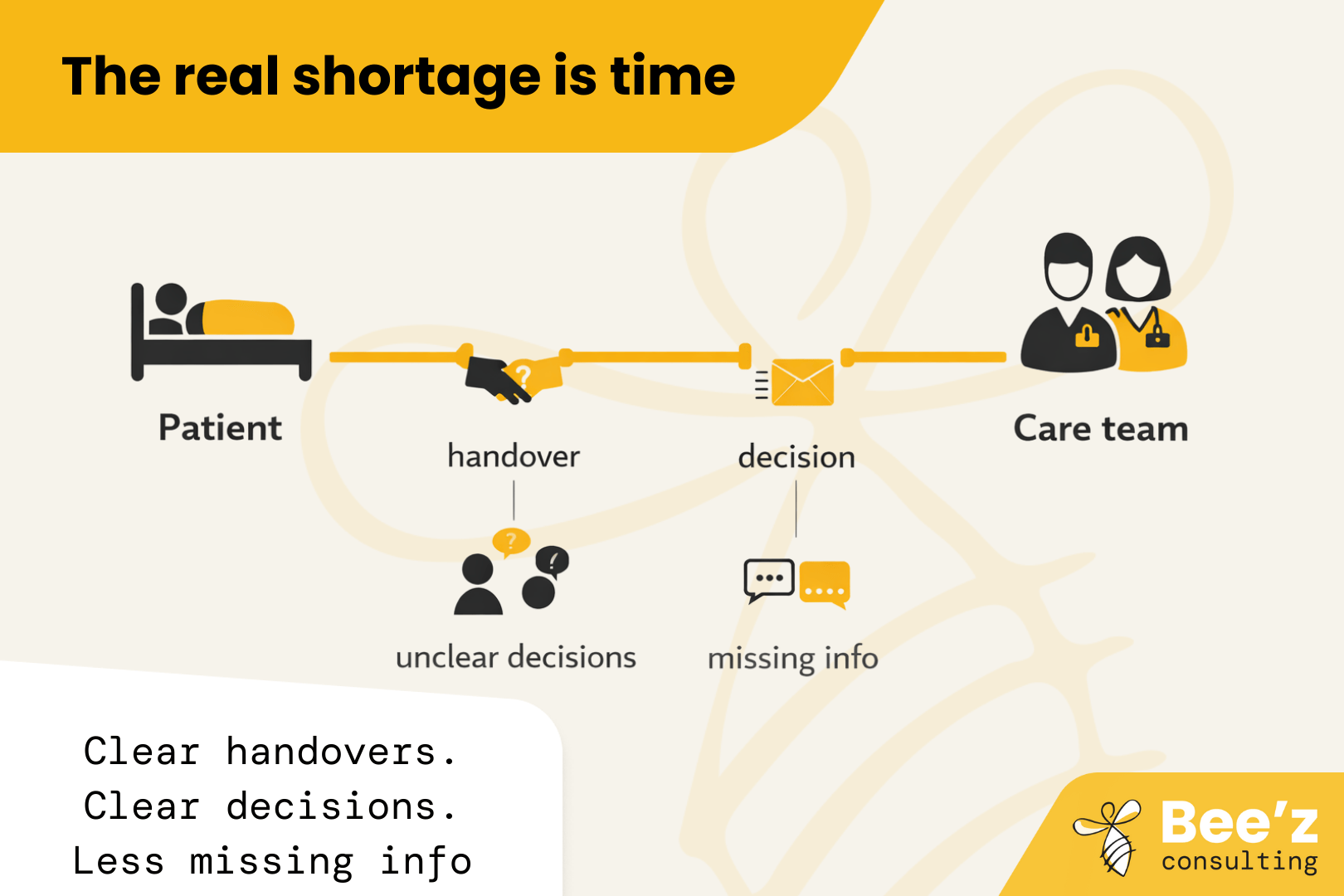
The real shortage is time with patients. “Thrive” is the missing lever. Fix daily workflow friction so hiring and retention finally pay off.
